GnRH antagonist protocol for ovarian stimulation during ART treatment: rFSH and hMG in the IVF

Ovarian stimulation in GnRH antagonist protocols
Poor ovarian response (POR) remains one of the major challenges for infertility clinics managing assisted reproductive technology (ART) treatments. The POR is characterized by a diminished response to ovarian stimulation by gonadotropins, which can occur either predictably or unpredictably. This condition typically results in a low yield of oocytes and consequently leads to reduced pregnancy rates1. For controlled ovarian stimulation (COS) in ART, GnRH analogues, including agonists and antagonists, are employed to suppress pituitary function. This suppression prevents premature luteinization by inhibiting the production of endogenous follicle-stimulating hormone (FSH) and luteinizing hormone (LH). A recent Cochrane meta-analysis indicates that live birth rates (LBRs) achieved using GnRH antagonist protocols are comparable to those obtained with long GnRH agonist protocols. However, GnRH antagonist treatments are associated with a lower incidence of ovarian hyperstimulation syndrome (OHSS) of any grade compared to GnRH agonist protocols. Consequently, based on current evidence, GnRH antagonist protocols are not only as efficacious as long GnRH agonist protocols but also off er a safer and more patient-friendly alternative2.
Several GnRH antagonist protocols are employed during COS in ART treatments, where the aim is to pharmacologically stimulate the ovaries to develop multiple ovarian follicles for the retrieval of multiple oocytes during follicular aspiration. These protocols typically utilize the most commonly available GnRH antagonists and can follow either a fixed or flexible regimen. In the fixed protocol, GnRH antagonists are generally introduced on Day 5 or 6 of COS. Conversely, the flexible protocol starts GnRH antagonists once the largest ovarian follicle reaches a specific size, usually between 12 and 14 mm, or when serum estradiol (E2) reaches a predetermined threshold3.
Both fixed and flexible antagonist protocols can be initiated with or without hormonal pre-treatment. This pre-treatment is employed by clinicians for various purposes, such as synchronizing follicular development, preventing early large follicles or spontaneous LH surges, reducing cyst formation, and scheduling in vitro fertilization (IVF) cycles to accommodate both clinical and patient needs, including the timing of oocyte retrieval4.
rFSH and hMG in the ART
Human menopausal gonadotropin (hMG) has both FSH and LH activities (in the form of LH and hCG, with short and long half-lives, respectively), and it may also have beneficial effects in terms of oocyte quality and endometrial receptivity similar to recombinant (rLH) supplementation5 .However, the largest meta-analysis, which included 4040 patients from 16 randomized controlled trial, found similar pregnancy rates between hMG and rFSH stimulation protocols5 .HMG produced less oocytes than rFSH and hMG protocols required higher total gonadotropin dose when compared with rFSH-only protocols.
In a study, researchers evaluated the effects of hMG administration, initiated either in the early or mid-follicular phase, on the outcomes of ART cycles in POSEIDON group 3 and 4 poor responders (n=558). In the study, hMG was commenced either at the early follicular phase or mid-follicular phase, while the control group did not receive hMG stimulation. The primary outcome measure was LBRs.
The results showed that the mean duration (± standard deviation) of stimulation was significantly shorter in the early follicular hMG group compared to the mid follicular hMG group (11.9 ± 3.6 days vs. 12.8 ± 4 days, respectively; p=0.027). The mean numbers of oocytes retrieved, and mature (MII) oocytes were similar across all groups. However, the LBRs per embryo transfer were significantly different among the groups, with rates of 21.9% in the early follicular hMG group, 11.7% in the mid-follicular hMG group, and 11.6% in the control group (p=0.035). Although the live birth rates were slightly higher in the POSEIDON group 3 patients than in POSEIDON group 4 patients, the results did not show statistical significance (Figure 1).
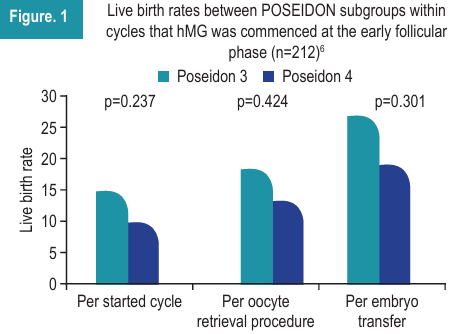
In conclusion, the study found a significant association between the timing of hMG initiation and live birth rates in ART cycles for POSEIDON group 3 and 4 poor responders. Early initiation of hMG, in combination with rFSH, appears to be beneficial for this specific population6.
In a study, researchers assessed the effect of controlled ovarian stimulation with rFSH plus rLH vs. hMG plus rFSH on fertility outcomes in IVF patients. The study compared clinical pregnancy outcomes in patients undergoing IVF/ICSI cycles using either hMG plus rFSH or rFSH plus rLH for controlled ovarian stimulation (COS). The findings suggest that the hMG plus rFSH regimen results in a greater number of embryos transferred, a higher clinical pregnancy rate, and ultimately a higher LBRs compared to the rFSH plus rLH regimen7.
In a study by Yang C et al. rFSH treatment was characterized by a higher number of retrieved oocytes (13.3) and transferable embryos (5.0), a higher fresh embryo transfer rate (35.0%), and multiple birth rate among the fresh embryo transfer cycles (8.2%). The pregnancy rate (32.7%) and LBR (25.5%) per transfer cycle (p>0.05). The cumulative LBR per started cycle with rFSH-alfa was 53.5%, rFSH-alfa was independently associated with a high cumulative LBR8 .According to the researchers, rFSH-alfa might achieve high transferrable blastocysts and cumulative LBR per started cycle.
Summary
- POR is a significant challenge in ART treatments, characterized by a diminished ovarian response to gonadotropins, leading to a low yield of oocytes and reduced pregnancy rates.
- GnRH antagonist protocols in COS for ART are as effective as long GnRH agonist protocols in terms of LBRs but are associated with a lower incidence of OHSS, offering a safer and more patient-friendly option.
- Early initiation of hMG during COS significantly shortened the mean stimulation duration compared to mid-follicular initiation with similar numbers of oocytes retrieved and matured across groups.
- The LBRs per embryo transfer have been shown to be markedly higher in the early follicular hMG group compared to the mid-follicular hMG group, indicating a significant benefit of early hMG initiation in ART cycles for POSEIDON group 3 and 4 poor responders
- Researchers have shown that rFSH treatment resulted in high numbers of retrieved oocytes and transferable embryos, with a higher rate of fresh embryo transfers and multiple births.
References
- Tarlatzis BC, Zepiridis L, Grimbizis G, Bontis J. Clinical management of low ovarian response to stimulation for IVF: A systematic review. Hum Reprod Update. 2003;9:61–76.
- Al-Inany HG, Youssef MA, Ayeleke RO, et al. Gonadotrophin-releasing hormone antagonists for assisted reproductive technology. Cochrane Database Syst Rev 2016;4:CD001750.
- Venetis CA, Storr A, Chua SJ, et al. What is the optimal GnRH antagonist protocol for ovarian stimulation during ART treatment? A systematic review and network meta-analysis. Hum Reprod Update. 2023;29(3):307–26.
- Farquhar C, Marjoribanks J, Brown J, et al. Management of ovarian stimulation for IVF: Narrative review of evidence provided for World Health Organization guidance. Reprod Biomed Online 2017;35:3–16.
- Lehert P, Schertz JC, Ezcurra D. Recombinant human follicle stimulating hormone produces more oocytes with a lower total dose per cycle in assisted reproductive technologies compared with highly purified human menopausal gonadotrophin: a meta-analysis. Reprod Biol Endocrinol. 2010;8:112.
- Berker B, Sukur YE, Ozdemir EU, et al. Human menopausal gonadotropin commenced o early follicular period increases live birth rates in POSEIDON group 3 and 4 poor responders. Reprod Sci. 2021;28(2):488–94.
- Tehraninejad SE, Taghinejad FM, Rashidi HB, Haghollahi F. Controlled ovarian stimulation with r-FSH plus r-LH vs. HMG plus r-FSH in patients candidate for IVF/ICSI cycles: An RCT. Int J Reprod Biomed. 2017;15(7):435–40.
Yang C, Dong N, Li F, Ji Y, Pan Y, She H. The cumulative live birth rate of recombinant follicle-stimulating hormone alfa verse urinary human follicle-stimulating hormone for ovarian stimulation in assisted reproductive technology cycles. J Ovarian Res. 2022;15(1):74.

Hello, This is a comment
12345
Hello 22 nov 123
Hi
Hello
Hello 12345
Hello 22 noew
Djjdjdje
Helo
1234
1234
Helol
hasdgfjhg juashfgjuhwfu
hello test 21 nov
Sjjdkd sjdjjdkd
test Hello20
test hello
Test blog comment loader
Hello mobile test
test
hello
hello
hi
Hello
Hello test mobile 2