Optimizing IVF success rates with Menotropin therapy

Infertility and IVF treatment
Infertility is a global issue,1 60–80 million couples experiencing infertility each year2. The use of in vitro fertilization embryo transfer (IVF-ET) to treat infertility in couples seeking medical care has become increasingly common2,3. From 1991 to 2021, live birth rates per embryo transplanted have increased for patients in the following age groups: 7% to 25% for patients 35–37, 6% to 17% for patients 38–39, and 3% to 10% for patients 40–424. On the other hand, some patient groups have low conception rates because of their restricted ovarian response to ovarian stimulation (OS) during IVF5.
Individuals seeking IVF/assisted reproductive technology treatment are those experiencing infertility due to aging ovaries. These patients are also sometimes referred to as impending primary ovarian insufficiency (POI), impending premature ovarian failure (POF), or poor ovarian responders (POR). Because many patients delay getting pregnant until their late thirties or even beyond their forties, the prevalence of these individuals appears to be rising6. Up to 20% of women seeking fertility counsel are POR, defi ned as women who do not react with OS treatment5.
Enhancing clinical pregnancy rates continues to be a primary priority for researchers3. Therefore, there is a need to manage POR during IVF cycles with the use of ovarian stimulators such as Menotropin, which is discussed in detail in this review.
Importance of ovarian stimulation
The goal of ovarian stimulation for IVF is to generate a large number of eggs and embryos7. Ovarian response to OS, as indicated by the quantity of oocytes recovered, is a crucial component of IVF cycles and a separate determinant in treatment outcome8. This raises the total likelihood of conception for each cycle that is started by enabling embryo selection and repeated transfers using the extra embryos from a single OS.7 The ideal response following OS is thought to be between 10 and 15 follicles. Between 6% and 35% of people are thought to have POR8. Under constant progress, IVF technology has made controlled ovarian hyperstimulation (COH) a primary therapeutic strategy for inducing ovulation and producing an optimal number of mature oocytes1.
The most common class of drugs used for OS in IVF cycles is gonadotropins. However, it is crucial to exercise caution to ensure the safety and efficacy of the treatment. Rather than inducing ovarian hyperstimulation syndrome (OHSS), this treatment should assist in obtaining the minimal number of eggs required to generate viable embryos for transfer7.
Role of Menotropin in ovarian stimulation
Menotropins are a purified preparation of gonadotropins extracted from the urine of postmenopausal women. It consists of follicle stimulating hormone (FSH) and luteinizing hormone (LH). To achieve the required degree of LH-like biological activity, human chorionic gonadotropin (hCG) is occasionally added9. The endometrium’s receptivity and the quality of the embryos are enhanced by hCG driven LH activity10.
In the early stages of folliculogenesis, FSH is essential for follicular recruitment, whereas LH plays a role in ovarian steroidogenesis and is involved in physiological processes that facilitate the development of a suitable preovulatory follicle in the later stages of folliculogenesis. Thus, in women with primitive ovarian insufficiency, Menotropin provokes both the growth and development of ovarian follicles as well as the gonadic steroids9.
Decrease in early pregnancy loss rates with Menotropin
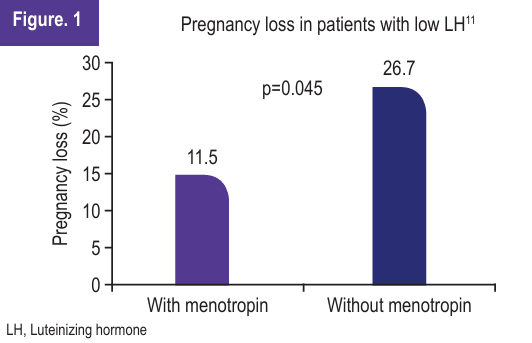
A single-centre, retrospective study was conducted by Yang A et al. to determine whether Menotropin supplement is associated with decreases in early pregnancy loss rates in patients exhibiting low endogenous LH during COS. Patients (n=110) who received Menotropin supplementation (Menotropin was initiated in conjunction with the GnRH antagonist at a daily dose of 75 IU for patients <55 kg and 150 IUs for patients ≧55 kg) were compared to those without Menotropin supplementation (n=174). The study focused on the number of implantation rates, pregnancy rates, and early pregnancy loss rates in both groups. The results of the study revealed.
- Patients who experienced low LH during gonadotropin hormone-releasing hormone (GnRH) antagonist protocol and supplemented with Menotropin were associated with lower early pregnancy loss when compared with patients without Menotropin supplementation (Figure 1).
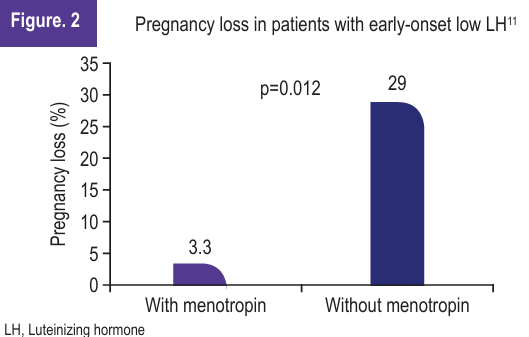
- In the sub-analysis of early-onset low LH group, the use of Menotropin was significantly associated with lower early pregnancy loss compared to patients in early-onset low LH group without the use of Menotropin (Figure 2).
- Other cycle outcomes for early-onset and late-onset low LH patients, though not statistically significant, were better with Menotropin use, as shown in Table 1.
| Table 1. Effect of Menotropin use on clinical outcomes in patients with early-onset and late-onset low LH 11 | ||||||
| Clinical variables | Early-onset low LH (n=131) | Late-onset low LH (n=153) | ||||
| Menotropin (n=63) | Non-supplemented (n=68) | p value | Menotropin (n-47) | Non-supplemented (n=106) | p value | |
| Blastocyst transfer cycles (%) | 25.4 | 20.6 | 0.539 | 21.3 | 17.9 | 0.658 |
| Implantation rate (%) | 29.1 | 24.1 | 0.403 | 29.5 | 21.6 | 0.195 |
| Clinical pregnancy rate (%) | 47.6 | 45.6 | 0.862 | 47.8 | 41.5 | 0.482 |
| Early pregnancy loss rate (%) | 3.3 | 29 | 0.012 | 25 | 22.7 | 0.999 |
| LH, Luteinizing hormone | ||||||
“Menotropin therapy was associated with a lower rate of early pregnancy loss in patients who displayed low LH during GnRH antagonist cycles11”.
Conclusion
- Infertility is a global issue, affecting millions of couples annually.
- Even though IVF increases the chances of conception for infertile couples, many patient groups have low rates of conception due to their limited ability to respond to OS during IVF.
- Menotropin, a purified preparation of gonadotropins consisting of FSH and LH, emerges as a promising option for managing POR during IVF cycles.
- Menotropin aided in follicular recruitment and ovarian steroidogenesis, a crucial process for successful IVF outcomes.
- Menotropin therapy was associated with a lower rate of early pregnancy loss in patients who displayed low LH during GnRH antagonist cycles.
References
- Bai L, Pan H, Zhao Y, et al. The exploration of poor ovarian response–related risk factors: A potential role of growth differentiation factor 8 in predicting ovarian response in IVF-ET patient. Front. Endocrinol. 2021; 12:708089.
- Katole A, Saoji A. prevalence of primary infertility and its associated risk factors in urban population of central India: A community-based cross-sectional study. Indian J Community Med. 2019;44(4):337–341.
- Giannelou P, Simopoulou M, Grigoriadis S, et al. The conundrum of poor ovarian response: From diagnosis to treatment. Diagnostics. 2020;10(9):687.
- Human Fertilisation and Emnryology Authority. Fertility treatment 2021: Preliminary trends and figures. [Internet].2023 June [cited 2024 Apr 09]. Available from: https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2021-preliminarytrends-and-figures/
- Polyzos NP, Camus M, Llacer J, et al. Corifollitropin α followed by menotropin for poor ovarian responders’ trial (COMPORT): A protocol of a multicentre randomized trial. BMJ open. 2013;3(6): e002938.
- Blumenfeld Z. What is the best regimen for ovarian stimulation of poor responders in ART/IVF? Front. Endocrinol. 2020; 11:485232.
- Duarte-Filho O, Miyadahira E, Matsumoto L, et al. Follitropin delta combined with menotropin in patients at risk for poor ovarian response during in vitro fertilization cycles: A prospective controlled clinical study. RB&E. 2024;22(1):7.
- Abu-Musa A, Haahr T, Humaidan P. Novel physiology and definition of poor ovarian response; clinical recommendations. Int. J. Mol. Sci. 2020;21(6):2110.
- Alviggi C, Conforti A, De Rosa P, et al. Drugs used for controlled ovarian stimulation. In Encyclopedia of Reproduction. 2nd Edition 2018.
- Smitz J, Platteau P. Influence of human chorionic gonadotrophin during ovarian stimulation: An overview. RB&E. 2020;18(1):80.
- Yang P, Wu M, Chao K, et al. Lower rate of early pregnancy loss in patients experiencing early-onset low LH in GnRH antagonist cycles supplemented with menotropin. JFMA. 2019;118(1):92–8.